Mobility difficulties due to spasticity, muscle weakness, and balance are the most common struggles among people who have cerebral palsy (CP). In the legs, orthoses can help people with CP in several ways, including helping to improve joint alignment, standing, and walking stability and reducing the risk of falls. In the arms, orthoses may be used to position and align the joints and improve function.
What is Cerebral Palsy?
CP is the most common motor impairment in childhood. It is a condition caused by damage to the developing brain and affects a person’s ability to control their muscles. The symptoms of CP vary from person to person. A person with severe CP may need to use special equipment to walk or may not be able to walk at all, while a person with mild CP may walk with little or no special help.
Orthosis Treatment Option
CP has no cure, but treatment can improve function and mobility. It is important to begin a treatment program as early as possible. Depending on the severity of CP and how it affects your child’s functional abilities, an orthosis may be recommended. An orthosis, also known as an orthotic device or brace, is an effective treatment option for those living with CP and experiencing spasticity, balance issues, coordination difficulties, and walking difficulties. Orthoses are external devices designed to support, stabilize, or correct various parts of the body. In the context of cerebral palsy, orthoses can be used to stabilize the joints to maintain alignment, improve balance, and improve a person’s ability to stand and walk around their environment, whether it might be at home, school, or work.
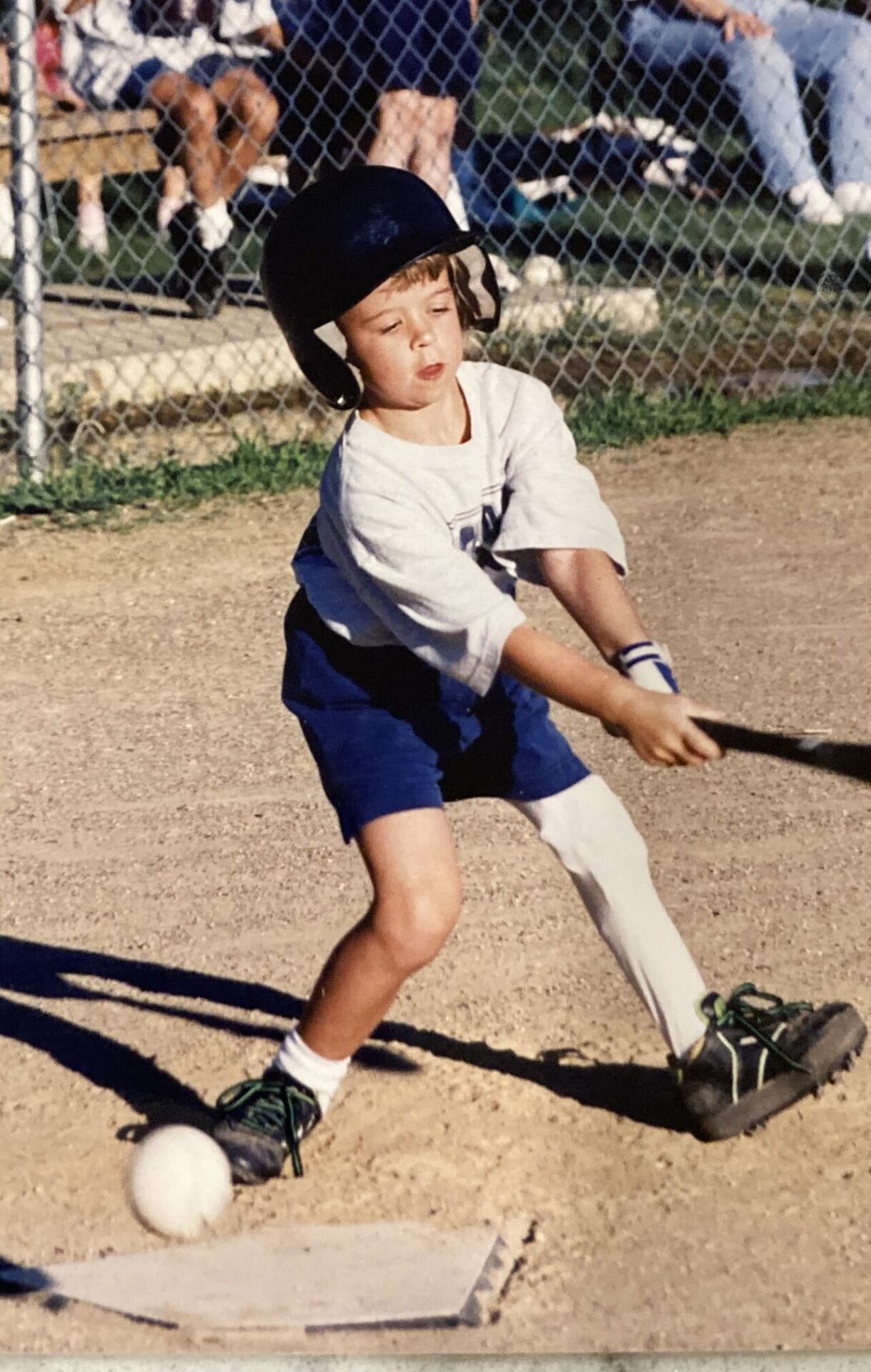
Mom to CP Warrior Shares Journey
Mom Jessica shares her daughter Abigail’s journey with cerebral palsy and how her orthotic leg braces have made a positive impact on her life.

Benefits of Wearing Orthosis for Cerebral Palsy
According to estimates, about two-thirds of children with CP can walk. However, CP affects the muscles, joints, and patterns of motion, meaning establishing a meaningful gait (walking pattern) can be a challenge. For example, one common condition is the tendency for children with CP to toe walk. This can be treated over time by using ankle-foot orthoses (AFOs) to help stabilize and strengthen the muscles and joints of the foot and ankle.
When an orthotic device is a successful part of treatment, it should help children establish more normal patterns of joint and muscle motion.1
1. Manage Spasticity
Because 80% of children with CP have spasticity, orthotic intervention can have a major effect on a child’s body mechanics.1 Spasticity is high muscle tone caused by involuntary muscle contractions. It can cause feelings of stiffness or tightness within muscles and a wide range of involuntary muscle spasms that can further impair movement and coordination.2 An orthosis can reduce the impact of spasticity by holding a part of the body in place to prevent unwanted movements and minimize spastic muscles from further tightening. Additionally, an orthosis may gently stretch tight muscles, which may help minimize spasticity progression. Once a stable basis for movement has been established, your child can develop higher levels of functioning, including increased range of motion, muscle strength, endurance, coordination, and step length.
2. Correct Posture
CP can cause low or high muscle tone or a combination of both. Low abdominal muscle tone may cause poor trunk stability, decreased balance, and compromised posture. On the other hand, high muscle tone may force the body into abnormal positions. Wearing a spinal orthosis can help provide stability and structural support to sit upright.
3. Decrease Pain
Spasticity can strain the musculoskeletal system, cause pain, disrupt sleep, affect mood, and hinder growth. Orthoses stabilize the joints and reduce muscle tightness, relieving excess pressure on the muscles, bones, and joints and helping reduce pain.
4. Minimize Irregular Growth
High muscle tone can pull the body into abnormal positions as a child grows. Deformities may develop when the muscles remain contracted or tightened for long periods during growth. Orthoses can help correct these abnormal positions.
5. Improve Functional Ability
CP generally requires more energy to perform movements, resulting in tiredness, which leads to increased irregular movements. Orthoses help stabilize and support the body, reducing fatigue and allowing more energy to be utilized toward better form.
6. Improve Self-Esteem
Orthoses help to maintain or improve mobility and function and free up time to focus on family, play, and pursuing interests. Most often, this allows those living with CP the opportunity to be more active and improve self-esteem.
Goals
There are many types of orthoses that may help, including foot orthoses (FOs), ankle-foot orthoses (AFOs), knee-ankle-foot orthose (KAFOs), spinal orthoses (TLSOs) and more. A Hanger Clinic orthotist can help to establish goals for your child’s lifestyle and activity levels. Typical goals may include improving muscle tightness, enhancing mobility, preventing falls, and improving coordination. An orthotist will work with your family and your care team to establish the best treatment option and provide care and support.
Request a Free Evaluation
If your child has been diagnosed with cerebral palsy and you are interested in learning more about orthotic bracing, schedule a free evaluation with one of our board-certified orthotists.
References