June is Scoliosis Awareness Month, which means it’s the perfect time to shed some light on the condition by answering parents’ frequently asked questions. To help set the record straight, we sat down with one of the nation’s leading scoliosis experts, Megan Chamis, MSPO, CO, who helped clarify everything from what it is to how it’s treated, and even what the treatment journey looks like for families who suddenly find themselves immersed in this whole new world of spine care.
Megan Chamis, MSPO, CO
Certified Orthotist, Hanger Clinic
Megan is an ABC-certified orthotist at Hanger Clinic in Hartford, Connecticut. With nearly 30 years of experience in treating adolescent idiopathic scoliosis, Megan is considered a nationally-recognized expert in the field.

Ask the Expert: Scoliosis and the Teenage Years
1. What is scoliosis?
In scoliosis, the bones of the spine shift and rotate from where the middle of the spine should be, causing it to curve. Although it can affect anyone at any age, it is most commonly diagnosed in the preteen and teenage years (ages 11-16) during growth periods.
2. What are the causes of scoliosis in adolescents?
The clinical term for scoliosis in preteens and teenagers is ‘adolescent idiopathic scoliosis.’ The word ‘idiopathic’ means there is no known cause.
3. How common is it?
Scoliosis is a fairly common condition affecting up to 5 percent of adolescents.1 It is more often seen in girls than boys and also tends to be more severe in girls than boys.1
4. How is scoliosis diagnosed?
Idiopathic scoliosis typically appears in otherwise healthy preteens and teens and is usually diagnosed by their pediatrician or after a regular scoliosis screening at school. The screening exam most commonly used is the Adam’s forward bend test, where the child bends over at a 90-degree angle with their arms hanging down. At this angle, signs of unevenness of the ribs/spine are visible.
If a child is thought to have scoliosis, the pediatrician will usually refer you to an orthopedic surgeon for x-rays and to determine the best course of treatment.
5. What are the signs of scoliosis?
Scoliosis curves often cause changes to the child’s posture, but it is usually not painful. Their head may be shifted to one side of the body, one shoulder may appear higher than the other, and unequal arm gaps on the sides of the body are typically noticed.
6. How do you treat scoliosis?
There are three proven treatments for scoliosis — observation, bracing, and surgery — depending on severity.
- Scoliosis curves less than 25 degrees are often observed by an orthopedic surgeon.
- When the curve is between 25-40 degrees on an x-ray and the child still has quite a bit of growing to do, the orthopedic surgeon may prescribe a scoliosis brace.
- If the curve is more than 50 degrees, the orthopedic surgeon may discuss surgery.
7. How does a scoliosis brace work?
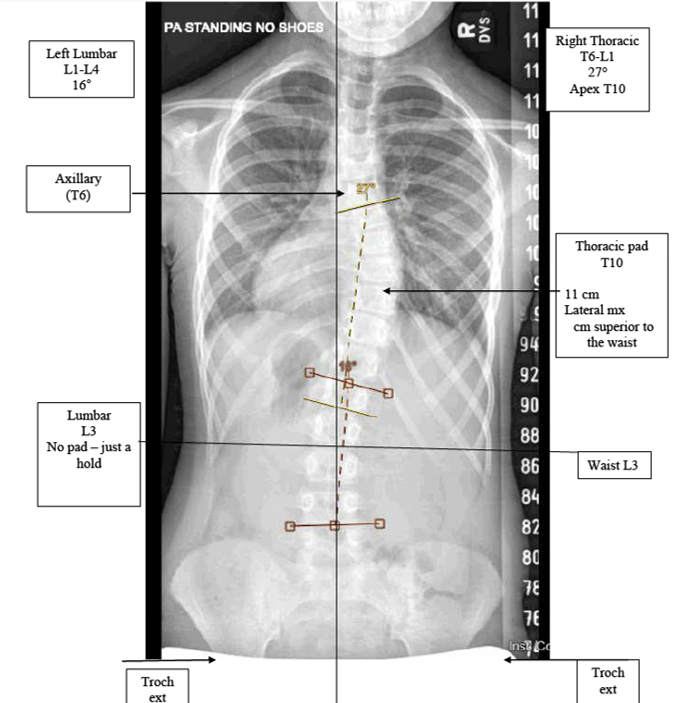
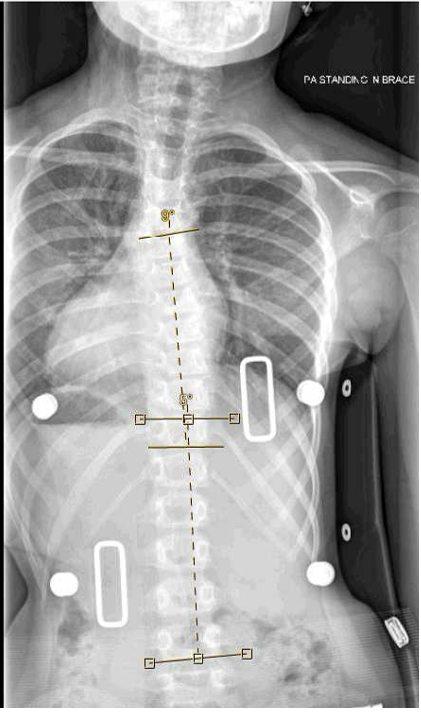
The scoliosis brace applies pressure over the back in specific areas to straighten the spine while the patient is wearing the brace. Usually, the spine will be corrected inside of the brace, but stay at the same degree of curve when the brace is removed. This is the primary goal of the brace — to stop the progression of the curve. So, if the child starts with a 27-degree curve, the goal is to keep the curve at 27 degrees and for it not to get worse over the course of treatment. It is important for families to understand that permanent straightening of the spine is not common and is not the goal of the brace.
8. How long do adolescents typically have to wear a brace?
Typical treatment timelines range from 1-3 years, with the most common timeframe being about 2 years. Since the timeline is usually quite long, brace compliance is key. In this case, compliance means wearing the brace for the number of hours indicated by the orthotist (the clinician who fits the brace). The orthotist will usually work with families to determine what is realistic in terms of wear time (taking into account sports, dance, activities, after-school commitments, etc.), so they can build a plan accordingly.
9. What is the difference between nighttime bracing and full-time bracing?
The referring physician will make the decision as to whether the child needs to be in a nighttime brace or a full-time brace based on several different factors (bone age, chronological age, onset of menstrual cycle [in girls], and curve magnitude).
The recommendation for nighttime bracing is to wear the brace 8-10 hours every night, and the recommendation for full-time bracing is to wear the brace 16-20 hours a day. There are numerous factors that influence the decision between full-time and nighttime brace prescriptions, with one key factor being compliance.
Studies show that full-time bracing worn greater than 17 hours had a much higher success rate of preventing the progression of the curve than in patients who wore their braces less than 17 hours, reinforcing the importance of brace compliance.2 Just as importantly, the nighttime brace will maximize the in-brace correction for fewer hours each day. The decision between full-time bracing and nighttime bracing is often discussed with the orthopedic surgeon, orthotist, patient, and family.
10. What can parents expect on the scoliosis bracing journey?
- The diagnosis is usually made by the child’s pediatrician or orthopedic surgeon, and the appropriate course of treatment is recommended.
- If the child’s curve is between 25-40 degrees, bracing will likely be prescribed and the referring physician will decide whether the child needs a nighttime brace or a full-time brace.
- The family will receive a prescription for the brace and will be referred to an orthotic provider, such as Hanger Clinic.
- At the first appointment (which typically takes 60-90 minutes), the orthotist will evaluate and measure the child for the brace indicated on the prescription. The evaluation consists of a clinical postural assessment looking at the shoulders, scapula, waist, and hips, as well as taking measurements and looking at the child’s x-rays. Measurements are typically taken either standing or laying down and sometimes even a scan is taken, so the orthotist can capture the shape of the child. At the same time measurements are being taken, the office staff will work to verify insurance coverage, with the goal of providing families with an understanding of their out-of-pocket costs (due to their deductible and coinsurance) prior to leaving the office or shortly thereafter.
- The orthotist will send the measurements and scans (if applicable) to a design center, where the brace will be fabricated.
- Within 2-3 weeks of the initial evaluation, families will return to the clinic for fit and delivery (this appointment typically lasts 60-90 minutes). At that time, the orthotist will evaluate and adjust the brace to ensure a comfortable fit and the proper function. At this time, they will review the break-in schedule and cleaning instructions, show the parent and child how to take the brace on and off, and will schedule the necessary follow-up appointments.

- The family will return 2-4 weeks later to assess the correction the child is getting in the brace (through an in-brace x-ray) and make necessary fine-tuning adjustments. The orthotist will also take the time to answer questions, break down barriers, and review wear time compliance. Compliance monitors are typically built into the braces, allowing the orthotist to print and review wear time reports with families, and celebrate the child’s accomplishments.
- The next follow-up appointment will be with their referring physician 4-5 months after the initial prescription was written, and they will continue to see their physician for follow-up appointments every 6 months throughout the course of treatment.
- Intermittently between the visits with their referring physician, families will see their orthotist for adjustments to accommodate for growth (typically every 3 months, depending on the type of brace and upon the discretion of the orthotist).
- Once the child has reached skeletal maturity (growth starts to slow down) and their referring physician feels the curve is stable, then bracing is discontinued.
11. What materials are the braces made of?
Typically, the braces are plastic on the outside and the majority of them are lined on the inside with foam (although the foam lining is optional to allow for a thinner aesthetic). Different color patterns are available for children who want to personalize their brace.
12. Are scoliosis braces uncomfortable to wear?
It usually takes 1-2 weeks for children to get used to wearing the brace, which is why orthotists allow for a gradual break-in schedule. While there may be areas of redness that correspond with the areas of pressure the brace is providing, there shouldn’t be blisters or sores associated with the bracing. The orthotist will advise on how to best address red spots based on the child’s individual case.
13. What is the best type of scoliosis brace for my child?
There are many different types and manufacturers of scoliosis braces available. The type of brace will be determined by the orthopedic surgeon as well as the expertise of the orthotist treating the child.
14. How long do scoliosis braces last?
Depending on the child’s growth, full-time braces last about 12 months and nighttime braces last anywhere from 18-20 months. This means that some children may require more than one brace over the course of treatment.
15. What sets Hanger Clinic apart in terms of clinical expertise?
We pride ourselves on our clinical expertise, which is why we established Clinical Practice Guidelines for treating adolescent idiopathic scoliosis. These guidelines serve as the standard of care at Hanger Clinic, and they include five different areas that help ensure Hanger Clinic clinicians treating scoliosis patients have the necessary experience and education to provide the best possible care and outcomes. They also define seven different biomechanical design considerations to ensure all braces provided through Hanger Clinic are fabricated to a certain, high-quality standard.
16. What advice would you give to parents just starting out on the scoliosis journey with their child?
My biggest piece of advice for parents would be to be patient with the process, ask the necessary questions and express concerns, and understand the goals of bracing and the longevity of treatment from the very beginning. We, as clinicians, understand that this isn’t an easy process and we want to be able to provide the emotional support needed every step of the way.
Request a Free Evaluation
Get started with the Hanger Clinic scoliosis treatment program at a location near you.

References
1. Konieczny, Markus Rafael et al. “Epidemiology of adolescent idiopathic scoliosis.” Journal of children’s orthopaedics vol. 7,1 (2013): 3-9..
2. Weinstein, Stuart L., et al. “Effects of Bracing in Adolescents with Idiopathic Scoliosis.” New England Journal of Medicine, vol. 369, no. 16, 2013, pp. 1512–21.

